 Why is it that superbly fit athletes can find themselves in as much back, knee, or neck pain as their flabby fans, who sit at desks all day long then watch sports from overstuffed sofas?
Why is it that superbly fit athletes can find themselves in as much back, knee, or neck pain as their flabby fans, who sit at desks all day long then watch sports from overstuffed sofas?
“When you do an activity over and over again, your body adapts to that activity,” warns Dr. Shirley Sahrmann, professor emerita of physical therapy at Washington University School of Medicine. “If you play tennis, your arm gets bigger on that side; if you do karate you get adaptations in your hip and leg. Even if you just sit, you lean, you slump, your neck goes forward.” Either your body fails to build up musculature to support itself, or it overbuilds certain muscles and throws off the symmetry your skeleton craves.
That’s why Sahrmann wants to see an annual physical therapy exam become as routine as a dental checkup. “We go to the dentist twice a year and spend thousands to straighten our teeth, and all we do with them is eat and talk. Meanwhile the rest of our body’s just hanging out there.”
People think of PT as something generic their doctor orders after an injury, she says. But by analyzing the way you walk, bend, sit, and carry yourself, physical therapists can prevent injuries and head off future surgeries and chronic pain.
“Kids don’t sit correctly, they slump, so they wind up sitting on the middle of their back,” she says. “We have these little bones on our bottom where we are supposed to sit and keep our spine erect. When you slump, the muscles get stretched out, and they’re not going to function optimally.”
A temporary phase? Maybe. But “bones adapt to the alignment that you keep them in,” Sahrmann points out, “and your spine becomes shaped like that.”
Watching teenagers walk makes her crazy: “They are not using what we consider a normal gait. They walk without bending at the hip and knee and pushing off. They shuffle. And they sway back—their shoulders are behind their hips—so their gluteal muscles don’t work as much as they should. All of these little cultural changes in sitting posture, what’s considered cool—even the clothing.” For a while there, she says, “the new waistline was the gluteal fold! And how do you walk when your legs are strapped together with a belt? Their knees get caught in the crotch of their pants—it’s hysterical. But it’s also not good.”
In years past, there was little appreciation of how lifestyle affected your health. “My family thought they just got diabetes or hypertension; it had nothing to do with the cans of Crisco my grandmother cooked with.” The way we move and align ourselves is just as important as what we eat, she says. “There is complexity to movement, and you can do it right or wrong.”
I bring up ergonomics—surely that’s helped? “It’s not just whether the setup is right,” she points out. “It’s what you bring to that setup and what you do when you’re not there.” We’re designed to keep changing position, not sit frozen in the perfect chair. Even working out requires real knowledge, if you want to lift weights or do aerobic training without compromising the performance of all your other joints.
Sahrmann’s one of the nation’s pioneers in pushing the concept of a movement system, emphasizing the subtle, necessary interconnections of muscles and bones and nerves but also heart, lungs, and the endocrine system. Her career has spanned more than half a century, and its twists and turns led her to see the body whole. She began work at the end of the polio era and spent nine years taking care of patients who’d suffered head injuries or strokes. In order to understand the disordered motor control of patients with central nervous system lesions, she left clinical practice to earn a Ph.D. in neurobiology. Then serendipity sent her a different kind of patient: athletes who had musculoskeletal pain. 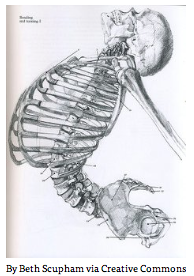
“I started teaching them to move differently, and they got better for reasons I didn’t understand,” she says. “I’ve spent a good many years with my colleagues at Wash.U. working to analyze these relationships between movement and musculoskeletal pain.”
She’s written two books and talked herself hoarse, urging people to see the body’s movement as systemic. Now that approach is finally catching hold, not just here but nationally and internationally. But she’ll know she’s really succeeded when PT evaluations are annual, and there are formal diagnoses based on movement patterns that consistently cause pain: flexion syndrome, when the back bows out; extension syndrome when it bows in and hunches you over; tibiofemoral rotation that can lead to knee problems.
“We all move differently,” she says. “I’ve seen patients whose feet are so callused I don’t know how they put their shoes on, and I’ve seen marathon runners with no calluses at all.
“You need to have an exam by a body expert at least once a year,” she finishes crisply. “Even if insurance doesn’t cover it, the cost is no more than you’d pay a personal trainer. I think we could substantially reduce the number of injuries and slow the process of osteoarthritis as people age.” She’s not saying arthritis can be eliminated altogether—but it can be delayed and its effects minimized. “There’s evidence that if a joint is lax, or you have injury, or your muscles are weak, you can get these arthritic changes.” Move right, and you lower the chance of injury—whether you’re an Olympian or a couch potato.
By Jeannette Cooperman May 11, 2015 / St. Louis Magazine

